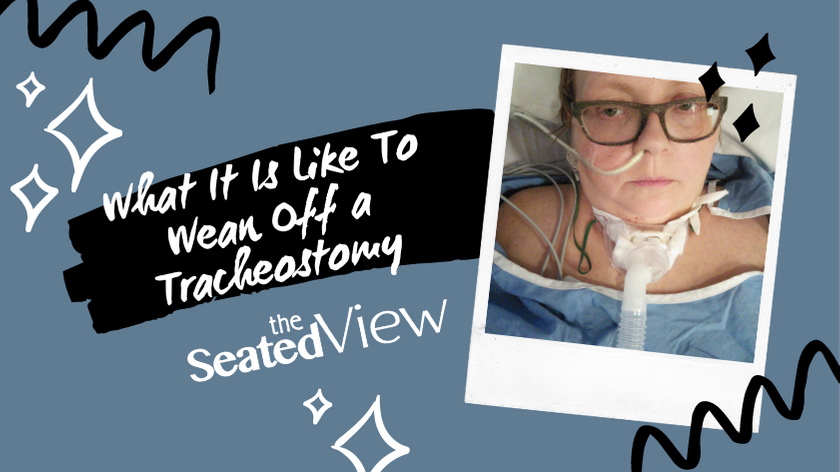
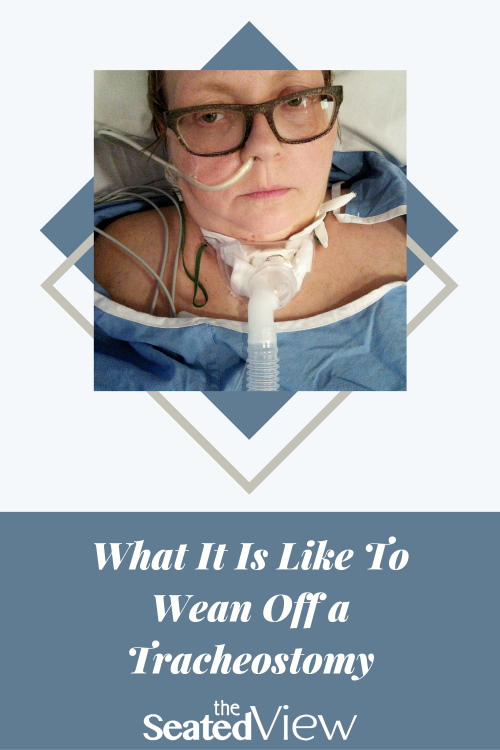
What It Is Like To Wean Off a Tracheostomy
Updated December 6, 2020
Trigger warning: medical trauma.
A quick recap: In March 2016, I got a bad flu, which developed into pneumonia. I ended up in the ICU in an induced coma and on a ventilator. Due to a bit of a mishap (understatement of the year) when being extubated, I had an emergency tracheostomy. Weaning off a tracheostomy and getting back to breathing on your own is a bit of a process.
In my previous post on what it is like to be on a ventilator, I wrote about the equipment that’s in your throat after a tracheostomy. A cuffed tube is inserted in the tracheostomy (i.e., a hole in your throat) and the cuff is inflated to make sure that the only air that’s is in your throat comes from the ventilator. Inserted into that tube is something called an inner cannula, which can be replaced as needed, for instance when the inner cannula gets gunked up (medical term, for realz) with lung secretions.
Eventually, you have to wean off both the ventilator and the trach. These tools have been really helpful while you were very sick, but ideally, you shouldn’t be on them for the rest of your life. The early stages of this process are little foggy for me — I had been very sedated and it took quite a while for me to get my brain back to the stage where wasn’t terribly fuzzy. I could be wrong about some of this, although I did consult The Boy on some of the details.

Weaning off the ventilator The first step to weaning off the ventilator is to decrease how much it’s breathing for you. Not too long ago, The Boy told me that most of the time, the ventilator was doing 60% of my breathing or thereabouts. When things were really bad, the ventilator was up at 100%, but let’s not talk about that.
One of the things that confused me was that although the ventilator was at a very low level and eventually off, I still had that tube in my trach. The tube was emitting humidified oxygen to help me breathe easier. One of the first stages of weaning off the ventilator is by wearing a mask on top of your trach. The mask is connected to the tube, so you still getting oxygen, but the ventilator is not breathing for you.
It is surprisingly tiring to breathe on your own after being on a ventilator and they start you out slow. I think my first session was an hour and a half. They increase to several sessions a day, each of them gradually longer. Once I was successfully able to breathe on my own for an extended time, I was officially taking off the ventilator, but still had the oxygen tube connected to the trach.
Weaning off the trach Almost all of the steps outlined below are scary. The actual medical procedure involved in several of them is not as bad as you’re convinced they are, but they involve your breathing and that’s where it gets unnerving. If you’ve been on a ventilator for a while, it feels sort of safe. Increasingly breathing on your own? That’s entirely different. But as I became fond of saying every time I moved on to another step, sooner or later, you have to jump in the deep end. So take a deep breath (!), hold someone’s hand, and go for it.
Deflating the cuff. About simultaneously with the beginning of the weaning process is the deflating of the cuff on the trach the tube in your throat, which makes it easier to breathe on your own.
This is also when I tried a speech valve., a little doohickey which is placed in the trach opening, enabling you to speak. This didn’t go too well for me. There wasn’t a lot of room in my airway because the trach equipment took up what space available in my supposedly small throat. It was much too much work to speak and after 10 minutes, I was drenched in sweat. So they took it out, but not before we did a recording of my weirdly robotic voice (the hissing is the oxygen).
I’d have to wait until further along in the process before I could speak again. The next steps would take place on the regular ward when I said goodbye to the ICU.
Fenestrated tube. Shortly after moving to a regular ward, they replaced the cuffed tube with the one that didn’t have a cuff and which was fenestrated. That means there was holes in the tube that went into the tracheostomy, creating more room for air to move through. It was an interesting process. My bed was flattened out and they popped out the hardware. I’d been dreading this — the thought of having people rooting around in my throat while I was fully conscious scared be bejesus out of me, but it turned out not to be too bad.
And then came the exciting part.
Corking. If everything’s gone well, the next step is corking. This is a totally charming name for something very obvious. They put a cap on the hole in the tube going into your throat, which means you are breathing fully on your own through your mouth and nose, instead of your throat. I was really excited to be able to blow my breath out through my mouth again for the first time in about a month. I spent several days doing this quite a lot.

And something even more exciting happened: being corked enabled me to speak again. I didn’t sound quite like myself — there was a plasticky sound to my voice and I only had enough breath for short sentences. But it was speech. Finally!
As with the ventilator mask mentioned above, corking takes place in sessions that gradually increase. You’ll still be encouraged to cough to clear your lungs of any residual gunk. Don’t be surprised if the cork flies off. Mine did. Several times.
And then comes the next really exciting part!
Decannulation. This is a very fancy word for getting the trach out. First, I went to the ENT clinic with a resident who put a scope up my nose and into my throat to assess my vocal cords. That’s not nearly as terrible as it sounds. Mainly, just makes you feel a strong urge to sneeze without actually sneezing. My vocal cords were still a little swollen, but air moved through them just fine. A couple of hours later, a respiratory therapist came to my bedside, popped off the trach equipment, and put a large square Band-Aid on top of the stoma (hole) in my throat. And yes. Of course I have a photo of what that hole looked like, I’ll leave it up to you whether to share it – are you game or are you squeamish? Leave your vote in the comments!
Breathing. Just a few hours after getting decannulated, The Boy and I were sitting on a quiet floor looking at a view of the city. I took a deep breath and realized that I hadn’t been aware of my breathing for quite a while. It was astonishing! And it made me realize how much work breathing had been with all that stuff in my throat. So quickly going back to breathing being effortless and just happening in the background was a true gift. I promised myself that I wouldn’t forget what that felt like, but it didn’t take too long of breathing normally before it just happened in the background.
Throat farts. The tracheostomy is left to heal on its own without sutures. There’s a bandage on top of it and you are instructed to put your hand against this stoma when you talk or cough. This will help it heal quicker — if you don’t, the wound gets opened up a little bit every time you cough or talk.
They don’t tell you about the throat farts, though. As long as the hole remains in your airway — and it can take anywhere from a few days to a few weeks or months to heal, depending on how long the trach was in — air will escape when you move, talk, or cough. It has to go somewhere and seeks the path of least resistance, i.e., out the sides of the bandage. This sounds remarkably like farting and I found it endlessly amusing.
If you can hold your hand against the bandage, the farting lessens. I couldn’t do that, so the spoon I’d used for a number of other things (push up my glasses, operate the buttons for adjusting the bed in the hospital, etc.) turned out to be really handy in this respect, too. I was back home by then and it got me some weird looks on the street as I held a wooden spoon against my throat. I thoroughly enjoyed bringing a touch of the surreal to people’s lives.

Although the tracheostomy has healed, it took a while before I got my normal amount of breath aback. It improve quickly, so it was just a matter of building up stamina. I thoroughly enjoyed being able to talk as much as I wanted, but my voice got hoarse easier than before.
Not surprisingly, this did not keep me from talking, though.
Tag: ARDS, asthma, coma, coming off ventilator, covid19, H1N1 influenza, ICU, induced coma, rheumatoid arthritis, trach, tracheostomy, ventilator, weaning off ventilator
6 Comments
Read More
Discover what else I've been writing about...









Thank you for writing this Lene, I had no idea how this worked. I am so glad you are doing better. You had us so worried.
I'll echo Rick and say thank you. I have a friend who lived with a permanent trache and I always wanted to ask her questions but rarely did. She passed when I was still new at being a lupus patient, so, it's been awhile. But I remember her putting her finger on her throat and gulping a deep breath every time she needed to speak.
This was just fascinating, Lene–I had no idea how complicated the whole process was. I'm sorry you had to go through the experience, but very, very glad it saved your life! I know your second book is still out there somewhere, and I want a copy! ;o)
I wouldn't mind seeing the photo of the “hole”, but I'm not squeamish about such things. Have at it!
Sending a warm hug, m'dear. :o)
As always you did wonderful job explaining a very difficult process. THANK GOD you are still with us I do! Glad your voice is getting stronger.
The effort involved!
Loved your interspersed pics. I suppose enough time has passed to be able to laugh –or guffaw, or croak….
Thank you for sharing your story. I needed a better understanding from someone who experienced this long journey! God Bless