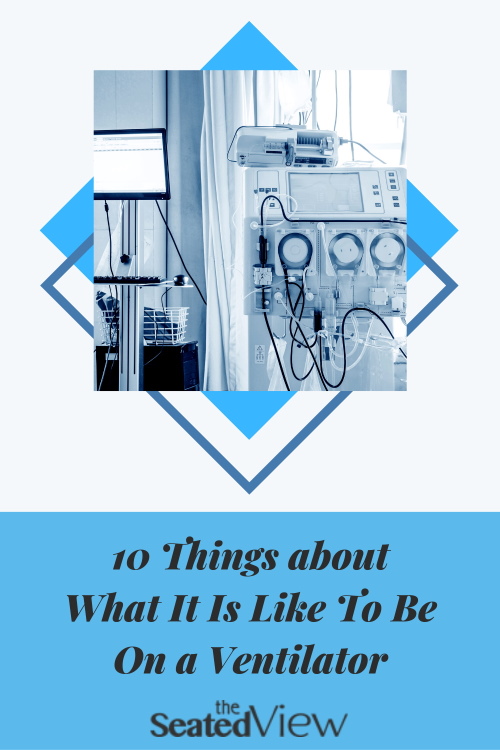
10 Things about What It Is Like To Be On a Ventilator

Updated December 6, 2020
Trigger warning: this post is about medical trauma. This post is a look at the experience of being on a ventilator from the point of view of the person on the receiving end of the tube. This happened when I had complications to the flu and ended up in the ICU.(side note: get your flu shot!)
I was initially ventilated with a tube going into my airway through my mouth, but don’t remember what that was like — I was in an induced coma, as is the norm when you’re ventilated. When an attempt was made to remove the tube (called extubation), it didn’t work and I crashed, flatlining briefly. I found out later that up to 40% of people who are extubated will need to be re-intubated. When they attempted to do that, my vocal cords were so swollen — fairly common after being intubated — that they had to do a tracheostomy. My memories of being on a ventilator start then.
It was an extremely educational experience. Which makes it sound as if it was no big deal and that’s not the case at all. I was remarkably calm about it at the time, but that likely had something to do with the happy pills they feed you in the ICU. It’s a stressful situation to be in and I guess they learned that the patients do better if heavily medicated.
Rhythm. I don’t actually remember much about the way the ventilator breathed for me, except the rhythm. The little jerk of the oxygen hose attached to the equipment in my throat as the ventilator shifted from breathing in and out quickly became just part of how things were. Not having breath above the tracheostomy was a bit weird, though, but mostly in retrospect (see above re: happy pills).
Noise. Being on a ventilator is noisy. The hiss of the oxygen is, granted, white noise, but it is remarkably loud. It makes you realize how quiet your normal life can be.
Being silenced. Not having any breath go past your vocal cords means you can’t talk. Communicating can be very difficult as a remarkable number of people (including staff in the ICU) reallllly suck at reading lips. It can take 15 minutes to communicate something very simple, longer if you’re trying to crack a joke. Pen and paper can be very useful. Initially, I could barely lift my arms and my writing was illegible. Not being able to talk was the most frustrating part of it all. It added an element of not quite being part of the conversation and made it very difficult to advocate for myself.

Tubes, tubes, tubes. I remember being very conscious of the hose that connected me to the ventilator and the oxygen. Any time you move, it moves with you and it is very flexible. Still, I was hyperaware of where it was, afraid of it being disconnected. And then there is the catheter, the NG tube (see below) the PIC line, and the arterial line. It’s a lot of tubes.
Pop-offs. Occasionally the hose from the ventilator pops off. At first, this was really scary, but I eventually discovered that I could make do on room air until someone came to reattach the tube. In the ICU, that happens quickly. Staff are used to the pop-off and someone will come running when it happens.
Equipment. Initially, a cuffed tube is inserted into the tracheostomy. The cuff is a small balloon that can be inflated or deflated, depending on what stage in the weaning process you are (more on that in the next post). When you are on the ventilator, the cuff is inflated to block any other sources of air. There’s another separate tube within that is called the inner cannula. This can be changed when needed. Despite all this equipment in your throat, it is remarkably stealth in terms of how it feels. Occasionally, I’d have a bit of a sore throat, which I assume was based on the position of the inner cannula.
Secretions. That’s a medical term. I call it lung gunk. We all have stuff in our lungs that we cough up during the day without noticing. When you’re on a ventilator you need to pay a lot more attention to this. It’s important to develop a good cough because that will help you get off the ventilator more quickly. Until you do, the gunk will often gather in the inner cannula, meaning you will need to be suctioned and sometimes it will need to be replaced. It’s amazing how quickly you get used to someone popping this thing in and out of your throat.
I’m not sure how suctioning is done when the ventilator is inserted through your mouth, as I have few memories from that time. When it’s through a trach, a thin tube is inserted into the inner cannula. I very quickly learned to develop my cough so I could get what was called a “tip section” in which the tube is inserted only an inch or so. Much deeper and it tickled my gag reflex and made me feel like I couldn’t breathe. It was worth it, though — being suctioned makes you feel much better and help you breathe more easily.
Feeding tube. Because your airway is occupied by equipment, you can’t protect it as well as you normally do. That means you get absolutely nothing by mouth. No food, no drink, and when you brush your teeth, the nurse will suction out whatever water might be in your mouth. Enter the NG (nasogastric) feeding tube, which is inserted through your nose and goes into your stomach (you don’t really feel it). You are hooked up to more or less a constant flow of liquid feed and your medications are crushed and injected into this tube. From the minute I woke up, I was fantasizing about drinking cold water — didn’t think much about food, but was desperate for water. When I arrived on the regular ward, the dietitian added a flush of the equivalent of a small cup of water every four hours. Feeling it come into my stomach was delightful.

Swallowing can be tricky. Not having eaten anything for a month weakens the muscles you use for swallowing. In order to be cleared for eating regular food you need a swallow test. They position you in front of an x-ray machine and record video of you swallowing a variety of foods on different points between liquid and solid. All of these foods are mixed with barium. Tasty! Over the next few weeks, I eased into eating, starting with soft foods, gradually adding more complicated items, such as crunchy things, food consisting of small bits (e.g., cereal), certain fruits, like oranges and apples, etc. Although my swallowing came back to normal fairly quickly, it took a while before I tackled popcorn or trail mix.
Dependency. One of the most profound feelings of being on a ventilator is the awareness that you are dependent on something else for your breath, the stuff that makes you live. Being in the ICU feels very safe — there is always someone around, nursing care is done one-on-one, or at most two patients to one nurse. You’re hooked up to a monitor that beeps an alarm if something is even slightly wrong. Once you move to a regular ward, this is not the case. Then you’re stuck in a room and need to press the call button to summon a nurse. It can take a while for it to be answered and for someone to come. Being on a ventilator on a regular ward is scary.
The good news about being on a regular ward is that it means you will continue the weaning process you started in the ICU and move towards decannulation (the equipment being taken out of your throat). More on that in the next post: What It’s Like to Wean Off a Tracheostomy.
Have you ever been on a ventilator or known someone who was? What was that experience like for you?
Edit: my memories are still a bit fuzzy and it turns out I was wrong about one aspect of this. The Boy has informed me that I was weaned off the ventilator by the time I was transferred to the regular ward. I remember that the hose attached to the wall was still attached to my trach, and that is true. However, by the time I went to the regular ward, it was not actively breathing for me, but merely a source of oxygen.
Tag: ARDS, asthma, covid19, flu, H1N1 influenza, ICU, pneumonia, rheumatoid arthritis, tracheostomy, ventilator
5 Comments
Read More
Discover what else I've been writing about...









That was very interesting to read. I have never been on a ventilator and hope not to. But I do find that medical professionals are horrible about describing how things feel because they have never had them themselves. Hence they say things like 'just a pinch' or 'you really won't feel a thing'. Hah! Thank you for sharing.
Thank you for writing this! I've wondered how these things work. All I know about trachs are from Father Mulcahey on M*A*S*H! And the time I had strep epiglottis and had a trach kit on my hospital bedtable all night, but didn't need it. No one explained anything, and I just went with my M*A*S*H memory! Ditto happy pills.
Oh, and on the subject of clueless, yet well meaning medical caregivers…they really shouldn't, when the ENT isn't returning his calls, repeatedly stop in the ER cubicle of the young mom sitting up, still as still can be, jaw jutting, barely breathing, like Darth Vader, and say “you need to take this more seriously! You have a life threatening condition!” Ok….good to know she was worried about me and the lack of the ENT. BUT, really not helpful! (Showed up finally. 1 hour of IV antibiotics and I was MUCH better!)
I have been on one (as you already know) but I was heavily sedated most of the time. I do remember being very unhappy and uncomfortable for the 2 days I was alert, even thinking to myself “I woke up for this????”. I had a very raspy voice afterwards. My then seven year old sons called me Lady Wolverine after the superhero.
Lene, I have often thought of you over the last few weeks. I have over the course of my life had to stand in a room with a vent. I have always wondered how it felt to be on the other end.
It is so good to have you back with us.
Take care!!!
Being on a ventilator sounds much less (in some ways maybe a little more) horrible than I imagined it to be. I know for sure that I'm very glad it was there to help you breathe so you could be here to tell us about it afterward, though. And love those amazing, smiling photos of you during your treatment. Honestly, people who have RD are the toughest, bravest people I know, and right now, you're at the tiptop of that list. I hope you get to try that popcorn soon!